Mental wellbeing and respiratory conditions
Research on wellbeing and COPD
The impact of psychological distress on lung function, disease exacerbation and mortality and health care resource utilisation is well documented.1 Due to the high prevalence of psychological distress in patients with COPD for example (Chetta et al 2005; van Manen et al 2002). how will this be properly screened, assessed and where appropriate treated.
There is growing research evidence that there are elevated levels of depression and anxiety in individuals with COPD and also in comparison with other chronic health conditions.2
From this research we know that psychological distress has a negative impact on an individuals physical symptoms of COPD. Quality of Life is also reduced. Levels of anxiety and depression are more highly correlated with quality of life than physical COPD symptoms.
The incidence of depression, in a recent longitudinal study by Schneider et al (n = 35,000, COPD) with a follow-up of 10 years was 16.2 cases per 1000 person-years in the COPD group compared to 9.4 cases per 1000 person-years in the non-COPD control group. In addition, those with severe COPD were twice as likely to develop depression compared to patients with mild COPD.
Over one third of individuals with COPD experience co-morbid anxiety and depression.3
Research on wellbeing and Asthma
Fatal and near fatal asthma has been associated with psychosocial dysfunction.4
Research on wellbeing and IPF
Increasing symptom burden in idiopathic pulmonary fibrosis patients leads to worsening mental health.5
What does this mean for patients?
Those suffering from depression are less likely to access other services which may be of benefit such as pulmonary rehabilitiation. There are recommended and effective treatments for anxiety and depression and as health and social care professionals we all have a responsibility to look after the emotional as well as the physical well-being of our patients/clients.
Listening and trying to understand what the persons respiratory condition means to them can help give us insight into how it may be affecting their mental wellbeing and what resources and support they have to deal with their condition. Obviously not all people respond in the same way to a diagnosis of respiratory disease and you may see a range of reactions as they adjust to what their respiratory condition means for them.
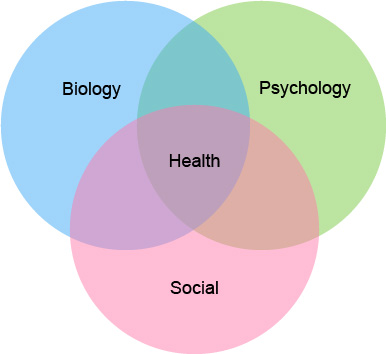
The biopsychosocial model of health can be a useful way of understanding all the factors that may influence our health and mental wellbeing. This model highlights the links between our biology, our physical health condition, our social circumstances and our psychological responses, what it means to us.6
Biopsychosocial model of health
| Health | ||
|---|---|---|
| Biology | Psychology | Social context |
|
|
|
References
- Felker et al 2001; McCathie et al 2002; Yohannes et al 2005; Ng et al 2007
- Abebaw M Yohannes and George S Alexopoulos European Respiratory Review 2014 Sep; 23(133): 345–349
- Panagioti M, Scott C, Blakemore A, Coventry PA (2014) Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 9:1289-1306.
- SIGN 153: British guideline on the management of asthma
- Katie Pink, Jack Boylan & Ben Hope-Gill (2013) A longitudinal study of anxiety and depression in idiopathic pulmonary fibrosis (IPF) European Respiratory Journal, 42 (Suppl 57) P2327.
- Engel, G.L., (1977). The Need for a New Medical Model: A Challenge for Biomedicine. Science, 196, 4286, 129-136
- Further reading
-
- Chetta A, Foresi A, Marangio E, et al (2005) Psychological implications of respiratory health and disease. Respiration 72 210-215.
- Felker B, Katon W, Hedrick S et al (2001) The association between depressive symptoms and health status in patients with chronic obstructive pulmonary disease. General Hospital Psychiatry 23 56-61
- McCathie H, Spence S and Tata R (2002) Adjustment to chronic obstructive pulmonary disease: The importance of psychological factors. European Respiratory Journal, 19 47-53.
- Ng TP, Niti M, Tan WC, Cao Z et al (2007) Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status and quality of life. Archives of Internal Medicine 167 (1) 60-67.
- van Manen JG, Bindels PJE, Dekker FW, et al (2002) Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax 57 412-416.
- Yohannes A, Baldwin R and Connelly M (2005) Predictors of 1-year mortality in patients discharged from hospital following acute exacerbation of chronic obstructive pulmonary disease. Age and Aging 34 491-496.




